ASCIA Guidelines - Acute Management of Anaphylaxis
![]() ASCIA HP Guidelines Acute Management Anaphylaxis 2024245.12 KB
ASCIA HP Guidelines Acute Management Anaphylaxis 2024245.12 KB
This document has been developed by ASCIA, the peak professional body of clinical immunology/allergy specialists in Australia and New Zealand. ASCIA information is based on published literature and expert review, is not influenced by commercial organisations and is not intended to replace medical advice. For patient or carer support contact Allergy & Anaphylaxis Australia or Allergy New Zealand.
ASCIA guidelines for the acute management of severe allergic reactions (anaphylaxis) are intended for medical practitioners, nurses and other health professionals who provide first responder emergency care. Appendix A includes additional information for health professionals working in emergency departments, ambulance services, and rural or regional areas, who provide emergency care.
Contents
- Definition and clinical diagnostic criteria for anaphylaxis
- Signs and symptoms of allergic reactions
- Immediate actions for anaphylaxis
- Anaphylaxis triggers and reaction times
- Adrenaline (epinephrine) administration and dosages
- Management of anaphylaxis in pregnancy and infants
- Positioning of patients with anaphylaxis
- Equipment required for acute management of anaphylaxis
- Supportive management and additional measures
- Actions after administration of adrenaline
Appendix A: Advanced Acute Management of Anaphylaxis
Appendix B: Acknowledgements
1. Definition and clinical diagnostic criteria for anaphylaxis
ASCIA defines anaphylaxis as:
- Any acute onset illness with typical skin features (urticarial rash or erythema/flushing, and/or angioedema), plus involvement of respiratory and/or cardiovascular and/or persistent severe gastrointestinal symptoms; or
- Any acute onset of hypotension or bronchospasm or upper airway obstruction where anaphylaxis is considered possible, even if typical skin features are not present.
The ASCIA definition is consistent with the following criteria published in the World Allergy Organisation Anaphylaxis Guidance Position Paper 2020.
Anaphylaxis is highly likely when any one of the following two criteria are fulfilled:
Criteria 1.
Acute onset of an illness (minutes to several hours) with simultaneous involvement of the skin, mucosal tissue, or both (e.g. generalized hives, pruritus or flushing, swollen lips-tongue-uvula), and at least one of the following:
a) Respiratory compromise (e.g. dyspnea, wheeze-bronchospasm, stridor, reduced peak expiratory flow, hypoxemia).
b) Reduced blood pressure or associated symptoms of end-organ dysfunction (e.g. hypotonia [collapse], syncope, incontinence).
c) Severe gastrointestinal symptoms (e.g. severe crampy abdominal pain, repetitive vomiting), especially after exposure to non-food allergens.
Criteria 2.
Acute onset of hypotension or bronchospasm or laryngeal involvement after exposure to a known or highly probable allergen for that patient (minutes to several hours), even in the absence of typical skin involvement.
2. Signs and symptoms of allergic reactions
Mild or moderate reactions (may not always occur before anaphylaxis):
- Swelling of lips, face, eyes
- Hives or welts
- Tingling mouth
- Abdominal pain, vomiting - these are signs of anaphylaxis for insect sting or injected drug (medication) allergy
Anaphylaxis – Indicated by any one of the following signs:
- Difficult or noisy breathing
- Swelling of tongue
- Swelling or tightness in throat
- Difficulty talking or hoarse voice
- Wheeze or persistent cough - unlike the cough in asthma, the onset of coughing during anaphylaxis is usually sudden
- Persistent dizziness or collapse
- Pale and floppy (young children)
- Abdominal pain, vomiting - for insect stings or injected drug (medication) allergy.
3. Immediate actions for anaphylaxis
- Remove allergen (if still present), stay with person, call for assistance and locate adrenaline injector.
- LAY PERSON FLAT - do NOT allow them to stand or walk
• If breathing is difficult allow them to sit with legs outstretched
• Hold young children flat, not upright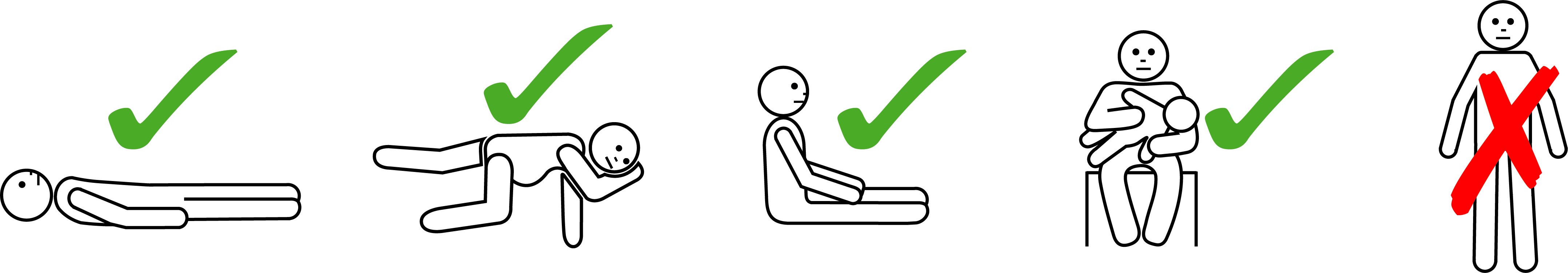
- GIVE ADRENALINE INJECTOR - Give intramuscular injection (IMI) adrenaline into outer mid-thigh without delay using an adrenaline autoinjector if available OR adrenaline ampoule/syringe. Adrenaline (epinephrine) is the first line treatment for anaphylaxis
- Give oxygen (if available).
- Phone ambulance - 000 (AU) or 111 (NZ) to transport patient if not already in a hospital setting.
- Phone family/emergency contact.
- Further adrenaline may be given if no response after 5 minutes.
IF IN DOUBT GIVE ADRENALINE
- Transfer person to hospital for at least 4 hours of observation.
- Commence CPR at any time if person is unresponsive and not breathing normally.
|
ALWAYS give adrenaline FIRST, then asthma reliever if someone with known asthma and allergy to food, insects or medication has SUDDEN BREATHING DIFFICULTY (including wheeze, persistent cough or hoarse voice) even if there are no skin symptoms. |
Note: If adrenaline is accidently injected (e.g. into a thumb) phone your local poisons information centre. Continue to follow this action plan for the person with the allergic reaction.
4. Anaphylaxis triggers and reaction times
The most common triggers of anaphylaxis are foods, insect stings and drugs (medications). Less common triggers include latex, tick bites, exercise (with or without food), cold temperatures, radiocontrast agents, immunisation (rare) and unidentified (idiopathic).
Anaphylaxis usually occurs within one to two hours of ingestion in food allergy. The onset of a reaction may occur rapidly (within 30 minutes) or may be delayed several hours (for example, in mammalian meat allergy and food dependent exercise induced anaphylaxis, where symptoms usually occur during exercise).
Anaphylaxis to stings and injected medications (including radiocontrast agents and vaccines) usually occurs within 5-30 minutes but may be delayed. Anaphylaxis to oral medications can also occur but is less common than to injected medications.
5. Adrenaline administration and dosages
Adrenaline is the first line treatment for anaphylaxis and acts to reduce airway mucosal oedema, induce bronchodilation, induce vasoconstriction and increase strength of cardiac contraction.
Give INTRAMUSCULAR INJECTION (IMI) OF ADRENALINE (1:1000) into outer mid-thigh (0.01mg per kg up to 0.5mg per dose) without delay using an adrenaline autoinjector if available OR adrenaline ampoule and syringe, as shown in the table below:
Adrenaline (epinephrine) dose chart |
|||
|
Age (years) |
Weight (kg) |
Volume (mL) of adrenaline 1:1,000 ampoules* |
Adrenaline injector devices (for use instead of ampoules) |
|
~<1 |
<7.5 |
0.1 mL |
Not available |
|
~1-2 |
10 |
0.1 mL |
7.5-20 kg (~<5yrs) 150 microgram device**
|
|
~2-3 |
15 |
0.15 mL |
|
|
~4-6 |
20 |
0.2 mL |
|
|
~7-10 |
30 |
0.3 mL |
>20 kg (~>5yrs) 300 microgram device***
|
|
~10-12 |
40 |
0.4 mL |
|
|
~>12 and adults |
>50 |
0.5 mL |
>50 kg (~12 years) 500 microgram**** or 300 microgram devices |
*Adrenaline 1:1,000 ampoules contain 1mg adrenaline per 1mL
**EpiPen® Jr is a 150 microgram (0.15 mg) device.
***EpiPen® is a 300 microgram (0.3 mg) device.
****Anapen® 500 is a 500 microgram (0.5 mg) device.
The adrenaline injector devices listed above are available in Australia and listed on the Pharmaceutical Benefits Scheme (PBS). EpiPen® and EpiPen® Jr are available in New Zealand (Pharmac listed since 2023).
Note:
- If multiple doses are required for a severe reaction (e.g. 2-3 doses administered at 5 minute intervals), consider adrenaline infusion if skills and equipment are available.
- For emergency treatment of anaphylaxis, ampoules of adrenaline 1:1,000 should be used for both IM doses and infusion if required (adrenaline 1:10,000 should not be used).
6. Management of anaphylaxis in pregnancy and infants
Management of anaphylaxis in pregnancy
Management of anaphylaxis in pregnant women is the same as for non-pregnant women. Adrenaline should be the first line treatment for anaphylaxis in pregnancy, and prompt administration of adrenaline (1:1,000 IM adrenaline 0.01mg per kg up to 0.5mg per dose) should not be withheld due to a fear of causing reduced placental perfusion. The left lateral position is recommended, as shown below. For more information go to www.allergy.org.au/hp/papers/acute-management-of-anaphylaxis-in-pregnancy
Management of anaphylaxis in infants
Whilst 10-20kg was the previous weight guide for a 150 microgram adrenaline injector device, a 150 microgram device may now also be prescribed for an infant weighting 7.5-10 kg by health professionals who have made a considered assessment. Use of a 150 microgram device for treatment of infants weighing 7.5 kg or more poses less risk, particularly when used without medical training, than use of an adrenaline ampoule and syringe.
Infants with anaphylaxis may retain pallor despite 2-3 doses of adrenaline, and this can resolve without further doses. More than 2-3 doses of adrenaline in infants may cause hypertension and tachycardia, which is often misinterpreted as an ongoing cardiovascular compromise or anaphylaxis. Blood pressure measurement can provide a guide to the effectiveness of treatment, to check if additional doses of adrenaline are required. The correct way to hold an infant is flat, as shown below.
7. Positioning of patients with anaphylaxis
- Fatality can occur within minutes if a patient stands, walks or sits suddenly.
- Patients must NOT walk or stand, even if they appear to have recovered.
A wheelchair, stretcher or trolley bed should be used to transfer the patient:
- To the ambulance and from the ambulance to the treatment room bed.
- From the treatment room bed to and from the toilet.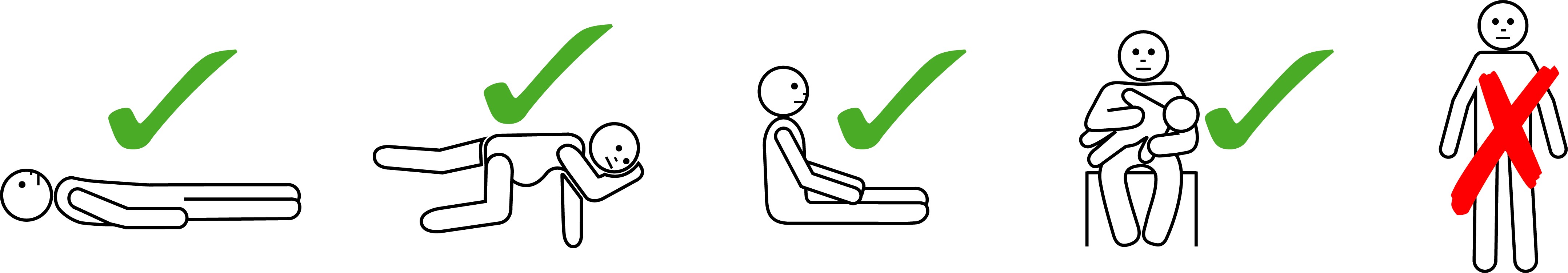
- Laying the patient flat (see image above) will improve venous blood return to the heart. By contrast, placing the patient in an upright position (standing or walking) can impair blood returning to the heart, resulting in insufficient blood for the heart to circulate and low blood pressure. This means that patients should not stand or walk, and this includes not being showered.
- If unconscious, vomiting or pregnant, lay the patient on their side in the recovery position.
-
The left lateral (recovery) position is recommended for patients who are pregnant (see image above). This reduces the risk of compression of the inferior vena cava by the pregnant uterus and improves venous return to the heart.
-
Patients with mostly respiratory symptoms may prefer to sit with their legs outstretched in front of them (see image above), which may help support breathing and improve ventilation. They should not sit on a chair as this may trigger hypotension. Monitor closely and immediately lay the patient flat if there is any alteration in conscious state or drop in blood pressure.
- The correct way to hold an infant or young child is flat (see image above), not upright nor over a shoulder.
- Do not allow the patient to stand or walk until they are haemodynamically stable, which is usually a minimum of 1 hour after 1 dose of adrenaline and 4 hours if more than 1 dose of adrenaline.
8. Equipment required for acute management of anaphylaxis
The equipment on your emergency trolley should include:
• Adrenaline 1:1,000 (consider adrenaline injector availability for initial administration by nursing staff)
• 1mL syringes; 22-25 G needles (25mm length) are recommended for IM injections for all ages* (consistent with Australian Immunisation Handbook). *Exceptions are preterm/very small infants (23-25G needle length 16mm) and very large adults (22-25G and needle length up to 38mm).
• Oxygen, airway equipment, including rebreather oxygen masks, nebuliser masks and suction
• Defibrillator
• Manual blood pressure cuff
• IV access equipment (including large bore cannulae)
• At least 3 litres of normal saline
• A hands-free phone in resuscitation room, to allow health care providers in remote locations to receive instructions by phone whilst keeping hands free for resuscitation.
9. Supportive management and additional measures - see Appendix A for additional information
Supportive management - when skills and equipment are available:
- Check pulse, blood pressure, ECG, pulse oximetry, conscious state.
- Give high flow oxygen if available and airway support if needed.
- Obtain IV access in adults and tachycardic and/or hypotensive children. The first sign of cardiovascular compromise in children is ongoing tachycardia. Hypotension can occur later, when it can then be difficult to get IV access, resulting in a significantly prolonged recovery process.
- If hypotensive, give IV normal saline 20mL/kg rapidly and consider additional wide bore IV access.
Additional measures - IV adrenaline infusion in clinical setting:
If there is an inadequate response after 2-3 adrenaline doses, or deterioration of the patient, start IV adrenaline infusion, given by staff trained in its use or in liaison with an emergency specialist.
IV adrenaline infusions should be used with a dedicated line, infusion pump and anti-reflux valves wherever possible.
CAUTION: IV boluses of adrenaline are NOT recommended without specialised training as they may increase the risk of cardiac arrhythmia.
Additional measures to consider if IV adrenaline infusion is ineffective
|
For upper airway obstruction |
|
|
For persistent hypotension/ shock |
|
|
For persistent wheeze |
Bronchodilators: Salbutamol 8-12 puffs of 100microgram (spacer) or 5mg (nebuliser). Note: Bronchodilators must not be used as first line medication for anaphylaxis as they do not prevent or relieve upper airway obstruction, hypotension or shock. Corticosteroids: Oral prednisolone 1 mg/kg (maximum of 50 mg) or intravenous hydrocortisone 5 mg/kg (maximum of 200 mg). Note: Steroids must not be used as a first line medication in place of adrenaline as the benefit of corticosteroids in anaphylaxis is unproven. |
Antihistamines have no role in treating or preventing respiratory or cardiovascular symptoms of anaphylaxis. Do not use oral sedating antihistamines as side effects (drowsiness or lethargy) may mimic some signs of anaphylaxis. Injectable promethazine should not be used in anaphylaxis as it can worsen hypotension and cause muscle necrosis.
10. Actions after administration of adrenaline
Observation of patient for at least 4 hours after last dose of adrenaline
Relapse, protracted and/or biphasic reactions may occur and overnight observation is strongly recommended if they:
- Had a severe or protracted anaphylaxis (e.g. required repeated doses of adrenaline or IV fluid resuscitation), OR
- Have a history of severe/protracted anaphylaxis, OR
- Have other concomitant illness (e.g. severe asthma, history of arrhythmia, systemic mastocytosis), OR
- Live alone or are remote from medical care, OR
- Present for medical care late in the evening.
True biphasic reactions are estimated to occur following 3-20% of anaphylactic reactions.
Adrenaline injector prescription and training
If there is a risk of re-exposure to allergens such as stings or foods, or if the cause of anaphylaxis is unknown (idiopathic) then prescribe and if possible dispense an adrenaline injector before discharge, pending specialist review. It is important to teach the patient how to use the adrenaline injector using a trainer device and provide them with an ASCIA Action Plan for Anaphylaxis which can be completed online and printed from the ASCIA website www.allergy.org.au/hp/anaphylaxis
Clinical immunology/allergy specialist referral
It is important that ALL patients who present with anaphylaxis are referrred to a clinical immunology/allergy specialist listed at www.allergy.org.au/patients/locate-a-specialist who will:.
- Identify/confirm cause.
- Educate about avoidance/prevention strategies and management of comorbidities.
- Provide ASCIA Action Plan for Anaphylaxis - preparation for future reactions.
- Initiate allergen immunotherapy where available (for some insect venoms).
- Refer to other relevant health professionals as required (e.g. dietitian).
ASCIA anaphylaxis resources
Management of anaphylaxis in the community (including the home, schools and children’s education/care) is facilitated by regular training and the use of an ASCIA Action Plan for Anaphylaxis, which includes instructions that are consistent with these guidelines.
To access ASCIA Action Plans and other anaphylaxis resources, including e-training courses, go to www.allergy.org.au/hp/anaphylaxis
Documentation of episodes
Patients should be advised to document episodes of anaphylaxis, and the ASCIA allergic reactions event record can be used to collect this information. www.allergy.org.au/hp/anaphylaxis/anaphylaxis-event-record
This facilitates identification of avoidable causes (such as food, medication, herbal remedies, bites and stings, co-factors like exercise) in the 6-8 hours preceding the onset of symptoms.
Patient and carer support
Patients should be referred to patient and carer support organisations for information on daily management and support whilst they await clinical immunology/allergy specialist review:
Allergy & Anaphylaxis Australia www.allergyfacts.org.au or Allergy New Zealand www.allergy.org.nz
Appendix A: Advanced Acute Management of Anaphylaxis
This additional information is intended for health professionals working in emergency departments, ambulance services, and rural or regional areas, who provide emergency care.
Supportive management (when skills and equipment available)
- Monitor pulse, blood pressure, respiratory rate, pulse oximetry, conscious state.
- Give high flow oxygen (6-8 L/min) and airway support if needed.
- Supplemental oxygen should be given to all patients with respiratory distress, reduced conscious level and those requiring repeated doses of adrenaline.
- Supplemental oxygen should be considered in patients who have asthma, other chronic respiratory disease, or cardiovascular disease.
- Obtain intravenous (IV) access in adults and in hypotensive children.
- If hypotensive:
- Give intravenous normal saline (20 mL/kg rapidly under pressure), and repeat bolus if hypotension persists.
- Consider additional wide bore (14 or 16 gauge for adults) intravenous access.
During severe anaphylaxis with hypotension, marked fluid extravasation into the tissues can occur: DO NOT FORGET FLUID RESUSCITATION.
Assess circulation to reduce risk of overtreatment
- Monitor for signs of overtreatment (especially if respiratory distress or hypotension were absent initially) – including pulmonary oedema, hypertension.
- In this setting (anaphylaxis) it is recommended that if possible a simple palpable systolic blood pressure (SBP) should be measured:
- Attach a manual BP cuff of an appropriate size and find the brachial or radial pulse.
- Determine the pressure at which this pulse disappears/reappears (the "palpable" systolic BP).
- This is a reliable measure of initial severity and response to treatment
- Measurement of palpable SBP may be more difficult in children.
Note: If a patient is nauseous, shaky, vomiting, or tachycardic but has a normal or elevated SBP, this may be adrenaline toxicity rather than worsening anaphylaxis.
Additional measures - IV adrenaline infusion
IV adrenaline infusions should only be given by, or in liaison with, an emergency medicine/critical care specialist.
If your centre has a protocol for IV adrenaline infusion for critical care, this should be utilised and titrated to response with close cardio-respiratory monitoring.
If there is not an established protocol for your centre, two protocols for IV adrenaline infusion are provided, one for pre-hospital settings and a second for emergency departments/tertiary hospital settings only.
It is important to note that the two infusion protocols have different concentrations and different rates of IV fluid infusion, resulting in the same initial rate of adrenaline infusion.
It is vital that IV adrenaline infusions should be used with the following equipment wherever possible:
- Dedicated line.
- Infusion pump.
- Anti-reflux valves in intravenous line.
Additional measures - IV adrenaline infusion for pre-hospital settings
If there is inadequate response to IMI adrenaline or deterioration, start an intravenous adrenaline infusion. IV adrenaline infusions should only be given by, or in liaison with, an emergency medicine/critical care specialist.
The protocol for 1,000 mL normal saline is as follows:
- Mix 1 mL of 1:1,000 adrenaline in 1,000 mL of normal saline.
- Start infusion at ~5 mL/kg/hour (~0.1 microgram/kg/minute).
- If you do not have an infusion pump, a standard giving set administers ~20 drops per mL; therefore, start at ~2 drops per second for an adult.
- Titrate rate up or down according to response and side effects.
- Monitor continuously – ECG and pulse oximetry and frequent non-invasive blood pressure measurements as a minimum to maximise benefit and minimise risk of overtreatment and adrenaline toxicity.
Note:
- This protocol is intended for temporary use, when no infusion pump is available.
- Most anaphylactic reactions settle with only 1 mg adrenaline in 1 litre.
- Indefinite continuation of low concentration infusion increases risk of fluid overload.
- Caution - Intravenous boluses of adrenaline are NOT recommended due to risk of cardiac ischaemia or arrhythmia UNLESS the patient is in cardiac arrest.
Additional measures: IV adrenaline infusion for emergency departments/ tertiary hospitals only
This infusion will facilitate a more rapid delivery through a peripheral line and should only be used in emergency departments and tertiary hospital settings.
The protocol for 100 mL normal saline is as follows:
- Mix 1 mL of 1:1,000 adrenaline in 100 mL normal saline.
- Initial rate adjusted accordingly to 0.5 mL/kg/hour (~0.1 microgram/kg/minute).
- Should only be given by infusion pump.
- Monitor continuously – ECG and pulse oximetry and frequent non-invasive blood pressure measurements as a minimum to maximise benefit and minimise risk of overtreatment and adrenaline toxicity.
Additional measures to consider if IV adrenaline infusion is ineffective
For persistent hypotension/shock:
- Give normal saline (maximum of 50mL/kg in first 30 minutes).
- In patients with cardiogenic shock (especially if taking beta blockers) consider an intravenous glucagon bolus of:
- 1-2mg in adults
- 20-30 microgram/kg up to 1mg in children
This may be repeated or followed by an infusion of 1mg/hour in adults.
- In adults, selective vasoconstrictors metaraminol (2-10mg) or vasopressin (10-40 units) only after advice from an emergency medicine/critical care specialist. Beware of side effects including arrhythmias, severe hypotension and pulmonary oedema.
In children, metaraminol 10 micrograms/kg/dose can be used. Noradrenaline infusion may be used in the critical care setting, only with invasive blood pressure monitoring.
Advanced airway management
- Oxygenation is more important than intubation.
- Always call for help from the most experienced person available.
- If airway support is required, first use the skills you are most familiar with (e.g. jaw thrust, Guedel or nasopharyngeal airway, bag-valve-mask with high flow oxygen attached). This will save most patients, even those with apparent airway swelling (these patients have often stopped breathing due to circulatory collapse rather than airway obstruction and can be adequately ventilated with basic life support procedures).
- DO NOT make prolonged attempts at intubation - remember the patient is not getting any oxygen while you are intubating.
If unable to maintain an airway and the patient's oxygen saturations are falling, further approaches to the airway (e.g. cricothyrotomy) should be considered in accordance with established difficult airway management protocols. Specific training is required to perform these procedures.
Special situation: Overwhelming anaphylaxis (cardiac arrest)
Key points:
- Massive vasodilatation and fluid extravasation.
- Unlikely that IMI adrenaline will be absorbed in this situation due to poor peripheral circulation.
- Even if absorbed, IMI adrenaline on its own may be insufficient to overcome vasodilatation and extravasation.
- Need both IV adrenaline bolus (cardiac arrest protocol, 1 mg every 2-3 minutes) AND aggressive fluid resuscitation in addition to CPR (Normal Saline 20mL/kg stat, through a large bore IV under pressure, repeat if no response).
- Do not give up too soon - this is a situation when prolonged CPR should be considered, because the patient arrested rapidly with previously normal tissue oxygenation, and has a potentially reversible cause.
Appendix B: Acknowledgements
A list of anaphylaxis references is available on the ASCIA website www.allergy.org.au/hp/anaphylaxis
The information in these guidelines is consistent with the following publications:
-
Acute Anaphylaxis Clinical Care Standard 2021, developed by Australian Commission on Safety and Quality in Health Care, in consultation with the Australasian Society of Clinical Immunology and Allergy (ASCIA), Allergy & Anaphylaxis Australia (A&AA), and the National Allergy Strategy (NAS). safetyandquality.gov.au/standards/clinical-care-standards/acute-anaphylaxis-clinical-care-standard
- Updated anaphylaxis guidelines: management in infants and children 2021 www.nps.org.au/australian-prescriber/articles/updated-anaphylaxis-guidelines-management-in-infants-and-children
- Anaphylaxis: emergency management for health professionals 2018
These guidelines are also based on the following international guidelines:
- World Allergy Organization (WAO) Anaphylaxis Guidance 2020 www.worldallergyorganizationjournal.org/article/S1939-4551(20)30375-6/fulltext
- American Academy of Allergy, Asthma and Immunology (AAAAI) Anaphylaxis - a 2020 practice parameter update, systematic review, and Grading of Recommendations, Assessment, Development and Evaluation (GRADE) analysis www.jacionline.org/article/S0091-6749(20)30105-6/fulltext
- International Liaison Committee on Resuscitation (ILCOR) and Australian and New Zealand Committee on Resuscitation (ANZCOR) Guidelines
© ASCIA 2024
Content and weblinks updated July 2024
For more information go to www.allergy.org.au/hp/anaphylaxis
To support allergy and immunology research go to www.allergyimmunology.org.au/donate
