 ASCIA PCC Eczema FAQ 2023129.5 KB
ASCIA PCC Eczema FAQ 2023129.5 KB
This document has been developed by ASCIA, the peak professional body of clinical immunology/allergy specialists in Australia and New Zealand. ASCIA information is based on published literature and expert review, is not influenced by commercial organisations and is not intended to replace medical advice. For patient or carer support contact Allergy & Anaphylaxis Australia or Allergy New Zealand. For more information visit the ASCIA website and the National Allergy Council Nip allergies in the Bub website.
Q 1: What is eczema?
Eczema is a chronic health condition that affects the skin, causing redness, dryness itching and sometimes infections. When eczema worsens it is called an eczema flare and usually there is no single factor for an eczema flare. Eczema flares can be triggered by a range of irritants (see Q 8) or for no obvious reason.
Eczema is also known as atopic dermatitis:
- Atopic conditions include eczema, allergic rhinitis (hay fever), dust mite and food allergy;
- It is common for people with eczema to have other atopic conditions.
- Unlike other atopic conditions, allergens do not usually directly cause eczema symptoms.
- Dermatitis is a general term for skin inflammation (redness and swelling).
Whilst a family history of allergy increases the tendency to develop eczema, the reasons why some people develop eczema is not well understood.
What is Eczema (Atopic Dermatitis)? https://ya.250k.org.au/eczema/ is a short animated video about eczema, that has been created as part of the National Allergy Strategy 250K youth project.
Q 2: What is the scratch and itch cycle of eczema?
The scratch and itch cycle of eczema can cause discomfort, disrupt sleep and affect quality of life:
- In people with eczema the skin does not retain moisture very well, which causes it to dry out easily.
- This makes the skin more open to allergens and irritants, which can trigger the skin to release chemicals that make the skin itchy.
- Scratching itchy skin causes more chemicals to be released, making the skin feel itchier.
- If eczema is well managed this can avoid the scratch and itch cycle. It is therefore important to keep skin that is prone to eczema well moisturised, by using moisturising creams on the skin every day.
Q 3: How does eczema affect people of different ages?
Eczema is a chronic health problem that affects people of all ages, but is most common in babies (infants):
- Infantile eczema occurs in around 20% of children under two years of age, and usually starts in the first six months of life. Infantile eczema usually improves significantly between the ages of two to five years.
- Childhood eczema may follow infantile eczema, or start from two to four years of age. Rashes and dryness are usually found in the creases of the elbows, behind the knees, across the ankles and may also involve the face, ears and neck. This form of eczema usually improves with age.
- Adult eczema is similar to that of older children with areas of very dry, itchy, reddened skin at the elbow creases, wrists, neck, ankles and behind the knees. It can cause rough, hard and thickened skin, which may also have weeping areas. Although eczema tends to improve in midlife, and is unusual in elderly people, it can occur at any age.
Q 4: Do people with eczema usually have other allergic conditions?
Many people with eczema have other allergic conditions. Studies have shown that up to 30% of babies with eczema who have a family history of allergy will develop food allergy, and up to 40% develop asthma or allergic rhinitis.
Q 5: How is eczema related to food allergy?
Whilst food allergy can trigger or worsen eczema symptoms in some people, food allergy is rarely the cause of eczema. Most food allergy causes hives (urticaria), vomiting and irritability within 30 minutes of eating the offending food. Food allergy only occasionally triggers delayed eczema flare ups.
Many babies with moderate or severe eczema will also have a food allergy. In some babies with severe eczema, short term removal of certain food/s using a medically supervised elimination diet may result in better eczema control. An elimination diet should be supervised by a clinical immunology/allergy specialist (or other medical specialist trained in allergy), in association with a dietitian with specialised knowledge of food allergies.
If there is no improvement in two weeks on the elimination diet, it means that food is unlikely to be the cause of the eczema. If the skin improves, foods are introduced one at a time as a medically supervised food challenge, to confirm which food causes the eczema to flare.
If food allergy is not the cause of eczema, removal of the food/s will not reduce symptoms.
Children with eczema and/or food allergy can have false positive allergy tests, and this can lead to unnecessary removal of foods which may affect growth and development. Removal of foods may also increase the risk of developing allergy to those foods. Therefore, allergy test results should always be interpreted by a clinical immunology/allergy specialist.
Q 6: How is eczema managed?
Eczema can be managed using the following steps, that are explained in detail in Q7-11:
- Maintain and protect skin every day.
- Avoid known triggers and irritants.
- Treat eczema flares and severe eczema.
- Control itch.
- Prevent and treat infection.
Q 7: How can skin be maintained and protected every day?
It is important to keep skin that is prone to eczema well moisturised every day:
- Moisturisers add moisture and form a barrier that protects the skin, so that it retains moisture. If the protective barrier of skin is damaged eczema frequently develops.
- Apply non-perfumed moisturiser to the face and body twice every day.
- Avoid moisturisers containing food proteins such as goat milk, wheatgerm and nut oils.
- After a bath or shower in lukewarm water, pat the skin dry and apply moisturiser.
- Use non-soap based wash or oil and avoid soap and bubbly products which dry out the skin.
- After swimming (especially in chlorinated pools), rinse and apply moisturiser.
Q 8: What triggers should be avoided?
People with eczema should avoid known triggers and irritants, which may include:
- Dry skin - this is one of the main triggers of eczema.
- Scratching - keep fingernails clipped (night gloves may be needed for young children).
- Viral or bacterial infections.
- Playing in sand, such as sandpits.
- Sitting directly on carpets or grass.
- Inhaling pollen allergens from grasses, weeds or trees in spring and summer.
- Irritants such as perfumes, soap and chemicals.
- Contact with animals, house dust mite allergen, wool and synthetic fabrics.
- Temperature changes, such as overly heated rooms.
- Stress, which can make eczema worse, although eczema is not a psychological condition.
- Constant exposure to water or chemicals, which can damage the protective barrier function of the skin.
Q 9: How should eczema flares and severe eczema be treated?
Skin damage can be prevented by applying creams or ointments prescribed by your doctor as soon as eczema is present. In contrast, not using enough of the treatments can cause skin damage due to itching, which can lead to scarring.
If prescribed, use topical corticosteroids or calcineurin inhibitors:
- These treatments actively treat inflammation (redness and itching).
- Ensure that adequate amounts are used. As a guide, one fingertip unit (FTU) is the amount of ointment from the first bend in the finger to the fingertip, which will cover an area equal to two adult hands.
- Apply moisturiser after corticosteroid cream or ointment has been applied.
If prescribed, use a recently listed treatment for severe eczema. There are now two treatments for severe eczema that are listed on the Pharmaceutical Benefits Scheme (PBS) in Australia for people aged 12 years or older with severe eczema which has not responded to other prescribed topical treatments:
- Dupixent® (dupilumab) is an immune modulating treatment given by injection that is self-administered. Dupilumab works by modifying the body’s immune response to prevent inflammation that plays a central role in eczema, but it is not an immunosuppressant.
- Rinvoq® (upadacitinib) is a Janus Kinase 1 (JAK1) inhibitor, that is taken as an oral tablet. JAK enzymes create signals in the body's immune system that result in inflammation, so JAK inhibitors work by blocking these signals. This reduces inflammation and the production of immune cells within the body.
It is important to ask your clinical immunology/allergy specialist or dermatologist to see if you are eligible for one of these treatments for severe eczema, which target different parts of the immune system.
Q 10: How can itch be controlled?
The following actions may reduce itch, to help control the scratch and itch cycle of eczema:
- Keep skin well moisturised every day.
- Use cold compresses and wet dressings/wraps, as directed.
- Consider using non-sedating antihistamines, especially if there are hives (urticaria). Sedating antihistamines are generally not recommended and should not be used in young children without specialist supervision.
Q 11: How can infections due to eczema be prevented and treated?
People with eczema that is not well managed can be more likely to have skin infections with bacteria such as Staph (Staphylococcus aureus), and viruses such as the cold sore (herpes simplex) virus.
People with eczema who have infections need to treat these as they occur. They may also need long term prevention strategies, such as diluted bleach baths, which can help prevent future skin infections.
Long term oral antibiotics can be helpful for people who suffer from recurrent infected eczema.
© ASCIA 2023
ASCIA is the peak professional body of clinical immunology/allergy specialists in Australia and New Zealand. For more information go to www.allergy.org.au
To support allergy/immunology research go to www.allergyimmunology.org.au
Content updated March 2023
![]() ASCIA Action Plan for Eczema 2024301.7 KB
ASCIA Action Plan for Eczema 2024301.7 KB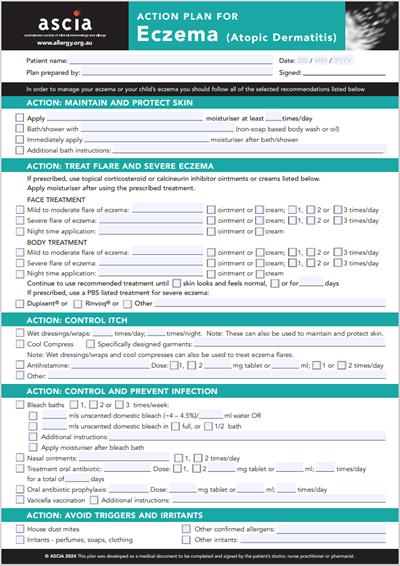

 Eczema (atopic dermatitis) affects the skin, causing redness, itching and sometimes infections. Eczema can usually be well managed by maintaining skin every day by applying moisturiser at least twice a day to the face and body, and avoiding known triggers or irritants.
Eczema (atopic dermatitis) affects the skin, causing redness, itching and sometimes infections. Eczema can usually be well managed by maintaining skin every day by applying moisturiser at least twice a day to the face and body, and avoiding known triggers or irritants.
 OFG results in swelling and inflammation of tissues, with clumps of many different types of white cells. The cause of OFG is unknown. While inflammation in OFG has been blamed on infections, there is no definite proof that OFG is due to any one infectious organism.
OFG results in swelling and inflammation of tissues, with clumps of many different types of white cells. The cause of OFG is unknown. While inflammation in OFG has been blamed on infections, there is no definite proof that OFG is due to any one infectious organism.