Checklist: Acute Urticaria and Chronic Urticaria
This document has been developed by ASCIA, the peak professional body of clinical immunology/allergy specialists in Australia and New Zealand. ASCIA information is based on published literature and expert review, is not influenced by commercial organisations and is not intended to replace medical advice.
For patient or carer support contact Allergy & Anaphylaxis Australia or Allergy New Zealand.
![]() ASCIA HP Acute Urticaria Chronic Urticaria 202583.07 KB
ASCIA HP Acute Urticaria Chronic Urticaria 202583.07 KB
The aim of checklist is to provide a summary of typical differences between acute urticaria (hives), which is a common, transient condition, and chronic spontaneous urticaria, to help guide management. It is important to differentiate between these conditions to determine the best approach to treatment.
|
Symptoms |
Acute Urticaria (New Onset), <6 weeks of symptoms |
Chronic Spontaneous Urticaria (CSU) |
|
Pruritic wheals appear anywhere on the body |
Yes: |
Yes: |
|
Severe symptoms that affect day to day function, leading to sleep disturbance, daytime tiredness, poor concentration. |
Rarely: |
Yes: |
|
Triggers |
Acute Urticaria |
Chronic Spontaneous Urticaria (CSU) |
|
Allergens, such as foods, drugs, insects, plants, pollens, dust mite, animal saliva. |
Sometimes: |
Rarely |
|
Infections and post-infections |
Yes: |
Sometimes |
|
Physical factors, such as heat, exercise, stress (cholinergic urticaria), cold temperatures (cold urticaria), alcohol and hormonal changes. |
Yes |
Yes |
|
Non steroidal anti-inflammatory (NSAIDS) medications |
Sometimes |
No |
|
Autoimmune conditions |
Less common |
Sometimes |
|
Idiopathic (unknown) |
Less common |
Sometimes |
|
Tests |
Acute Urticaria |
Chronic Spontaneous Urticaria (CSU) |
|
Skin prick tests or blood tests for allergen specific IgE) |
Not usually/rarely required: |
Not recommended: |
|
Other tests required for diagnosis |
Not usually/rarely required: |
Sometimes: |
|
Treatments and Referrals |
Acute Urticaria |
Chronic Spontaneous Urticaria (CSU) |
|
Trigger avoidance or minimisation |
Yes: |
Yes: |
|
Antihistamine tablets or syrups (non-sedating) |
Yes: |
Yes: |
|
Oral corticosteroids (short course) |
No |
Occasionally: |
|
Biologics |
No |
Yes: |
|
Referral to clinical immunology /allergy specialist recommended |
Not usually/rarely required: |
Yes: |
© ASCIA 2025
Content developed April 2025
For more information go to www.allergy.org.au/hp/skin (health professionals) or www.allergy.org.au/patients/skin-allergy (patients/carers)
To support allergy and immunology research go to www.allergyimmunology.org.au/donate


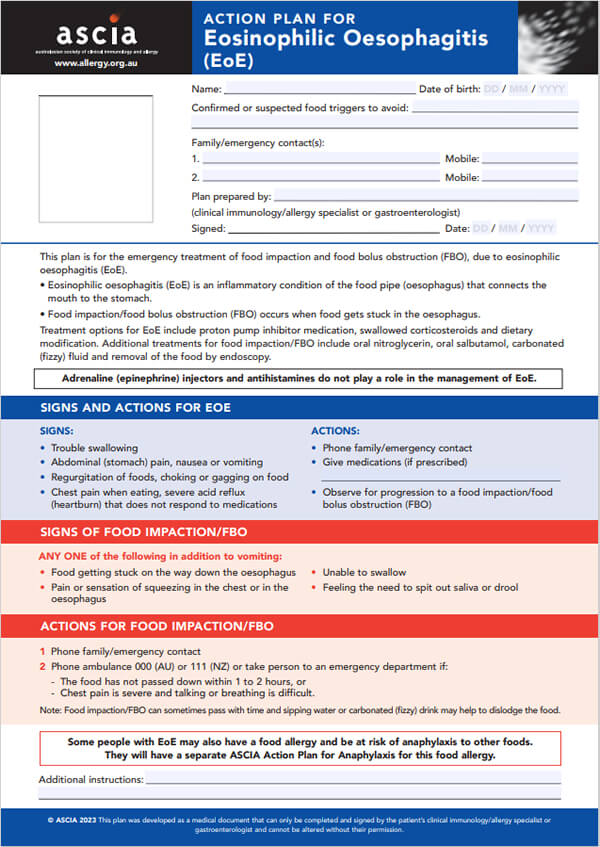
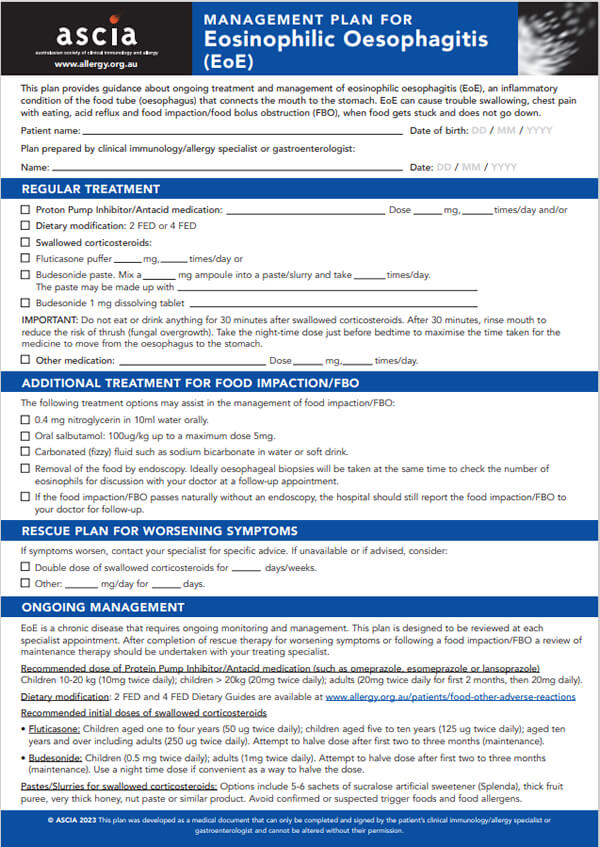
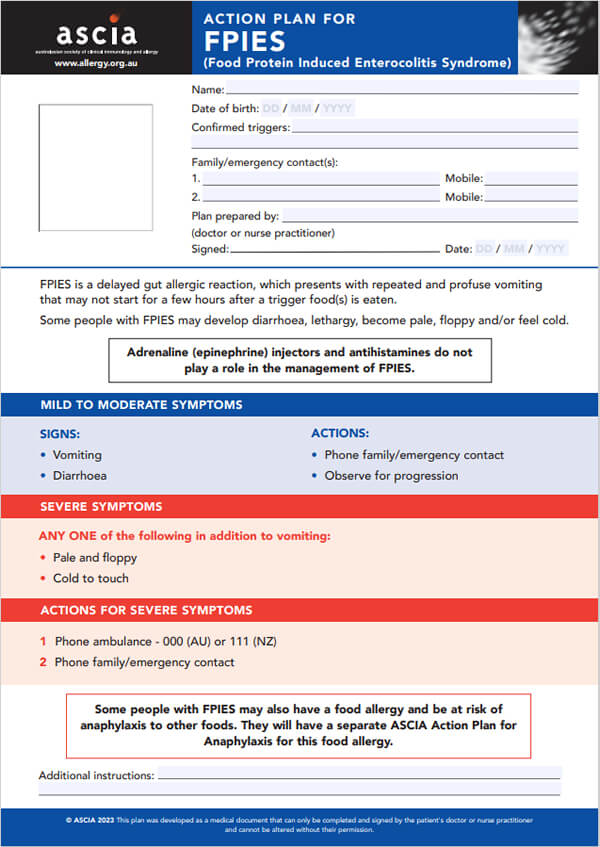
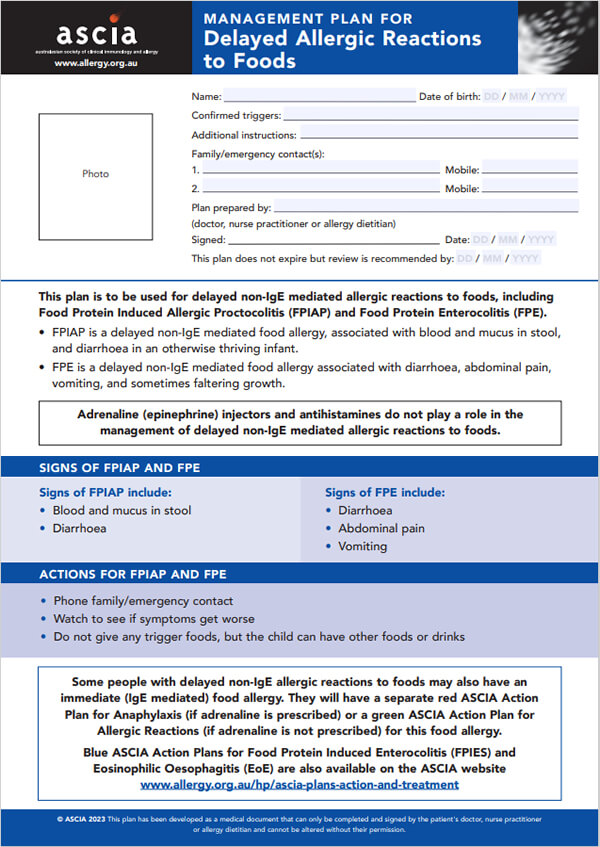
 Other adverse reactions to foods include eosinophilic oesophagitis (EoE), food protein-induced enterocolitis syndrome (FPIES), food protein induced allergic proctocolitis (FPIAP), food protein enterocolitis (FPE), oral allergy (food pollen) syndrome and food intolerances.
Other adverse reactions to foods include eosinophilic oesophagitis (EoE), food protein-induced enterocolitis syndrome (FPIES), food protein induced allergic proctocolitis (FPIAP), food protein enterocolitis (FPE), oral allergy (food pollen) syndrome and food intolerances.