 ASCIA PCC Pollen allergy 2022156.34 KB
ASCIA PCC Pollen allergy 2022156.34 KB
Pollen from grasses, weeds or trees can trigger symptoms of allergic rhinitis (hay fever), and asthma. Pollen seasons can last for several months and exposure is difficult to avoid. However, there are several ways to prevent or reduce pollen allergy symptoms.
What is pollen?
The word pollen is derived from the Greek word meaning 'fine flour' and the role of the pollen grain is to fertilise the female flower to reproduce plant species.
Pollen grains can be spread by birds, insects (bees, butterflies and moths), andwind:
- Some plants such as flowering plants, including wattle trees, produce small amounts of pollen which are distributed by birds and insects from one plant to another.
- Other plants such as pasture grasses and weeds, rely on wind to spread their pollen. These pollens are produced in large amounts, blow long distances and cause allergies in people, even if they live a long way from the source.
Most of the pollens that cause allergies are produced by airborne pollen from northern hemisphere grasses, trees and weeds:
- Improved pasture grasses are more allergenic than Australian native grasses.
- Pollen from exotic trees, which are planted for their autumn colour, is more allergenic than pollen from Australian trees.
Several types of weeds with highly allergenic pollen have been introduced to Australasia, including:
- Pellitory weed (also known as asthma weed), was accidentally introduced in a shipload of marble from Italy in the early 1900s. It is mainly found in Sydney.
- Paterson's Curse (Echium plantagineum) is a flowering plant that was deliberately brought from England in the late 1800's by Dr Paterson. It has taken over large areas of grass in rural Australia and produces highly allergenic pollen.
- Ragweed and Parthenium weed were introduced in pasture seed imported from the United States. They have spread throughout Queensland and northern New South Wales.
Pollen allergy causes allergic rhinitis
The correct name for hay fever is seasonal allergic rhinitis. Symptoms are caused by the body's immune response to inhaled pollen, resulting in chronic inflammation of the eyes and nasal passages.
Allergic rhinitis symptoms include:
- Runny, itchy, congested nose.
- Irritable, itchy, watery and red eyes.
- Itchy ears, throat and palate.
Allergic rhinitis is a common and debilitating disease
- Allergic rhinitis affects around 18% of people in Australia and New Zealand.
- Allergic rhinitis predisposes people to more frequent sinus infections.
- People with allergic rhinitis are often tired due to poor sleep quality.
- Moderate or severe allergic rhinitis can affect general health, impair learning, increase time off work, and reduce productivity.
- Around 80% of people with asthma have allergic rhinitis, which can make asthma difficult to control.
Pollen can trigger asthma
Pollen can directly trigger asthma and allergic rhinitis. Small particles of allergens can penetrate deep into the airways of the lung. Thunderstorms can also contribute to this:
- When pollen granules come into contact with water, starch granules are released that are small enough to be breathed into the airways, causing allergic rhinitis and asthma in some people
- People who wheeze during spring and/or summer, should see their doctor for advice.
Pollen seasons can last for months
In Australia pollen numbers are lower on the east coast where most winds come from the sea, and where there is protection from westerly winds by the Great Dividing Range. Pollen numbers are higher on the Victorian south coast because most winds are from the north carrying pollen from the northerly grasslands. In South Australia and Western Australia, the amount of pollen can vary according to the wind.
Pollination times vary with the plant variety and its location.
- Trees usually pollinate in late winter and early spring.
- White Cypress (Murray) Pine is the only Australian tree that produces highly allergenic pollen. It grows from the western slopes and plains of Eastern Australia across to Western Australia, south of the Tropic of Capricorn, and flowers from late July through to the end of August.
- Wattle trees are frequently blamed for early spring symptoms but tests raraely confirm that Wattle pollen is the cause.
- There are many species of Casuarina or Australian Oak trees, which produce pollen throughout the year and may cause allergic rhinitis symptoms at any time of the year.
- Grasses flower next, and the weed 'Plantain' flowers from August through to May.
The principal grasses growing in the northern coastal areas are subtropical and mainly flower in January, February and March. Allergenic grasses in the southern part of Australia are mostly Northern hemisphere grasses, with the main flowering period from October to December.
Diagnosis is important
A history should be taken of the timing of symptoms, identifying plants and trees that grow in the area, and if relief comes by going away on holiday. When the person's allergy history has been obtained, skin prick tests and/or blood allergen specific IgE tests, should be done using allergens that are in the area of their home and work. Test results can be interpreted by a doctor trained in allergy, in conjunction with the person's history.
Tips for reducing pollen exposure
- Stay indoors until after midday, particularly in the pollen season and on windy days.
- Avoid going out just before, during, or after thunderstorms, particularly when pollen counts are high.
- Wear sunglasses, carry tissues, shower when you arrive home, and rinse your eyes with water.
- Do not mow grass and stay inside when it is being mown. If mowing is unavoidable, wear a mask or take a non-drowsy antihistamine.
- Keep windows closed at home and in the car. Use recirculating air conditioning in the car.
- Do not picnic in parks or in the country during the pollen season.
- Try to plan holidays out of the pollen season or holiday at the seaside.
- If landscaping at home, research plants less likely to trigger allergic rhinitis or asthma. If you are sensitive to particular weeds or trees that are outside your bedroom window, have them removed.
Effective treatments are available
Seek advice from your pharmacist or doctor about medications that will relieve your symptoms. Although medications do not cure allergies, they are much more effective with few side effects. It is important to use them correctly, and to avoid medications that can cause problems such as frequent decongestant (unblocking) nose sprays or tablets.
Antihistamine tablets or syrups (non-sedating) help to reduce symptoms (sneezing, itchy and irritated eyes), but they are not as effective in controlling severe nasal blockage and dribble. The advantage of antihistamines is their flexibility; you can take them when you have symptoms, and avoid them when you are well. Antihistamine eye drops can also be helpful in controlling watery eyes due to allergies.
Intranasal corticosteroid nasal sprays (INCS) have a potent action on inflammation when used regularly (like asthma preventer medications). These need to be used regularly and with careful attention to the way in which they are used. Different brands of INCS vary in strength and effectiveness, so it is important to read the labels and check details with your pharmacist or doctor.
Combination medications containing an antihistamine and intranasal corticosteroid nasal spray are available and offer the combined advantages of both medications.
Decongestant sprays unblock and dry the nose, but should not be used for more than a few days as they can cause long term problems in the nose
Decongestant tablets unblock and dry the nose, but should be used with caution as they can have 'stimulant' side effects like tremors, trouble sleeping, anxiety or an increase in blood pressure. People with high blood pressure should not take decongestant sprays.
Natural products such as salt water nasal sprays or douches can be effective in relieving symptoms.
Appropriate management of pollen asthma includes commencing asthma preventer medication before, or at the first sign of asthma symptoms. Some people undergoing allergen immunotherapy for allergic rhinitis find that their asthma improves as well.
Allergen immunotherapy is a long-term treatment option
Medications only reduce the severity of symptoms and do not cure allergic rhinitis. Another treatment option is allergen immunotherapy (AIT) which is also known as desensitisation. AIT switches off the allergic reaction, by repeatedly introducing small doses of allergen extracts, by injection, sublingual tablets, sprays or drops.
AIT is a long term treatment which is usually given over a few years.
It should only be started after assessment by a clinical immunology/allergy specialist to determine if this is a suitable treatment option.
© ASCIA 2022
ASCIA is the peak professional body of clinical immunology/allergy specialists in Australia and New Zealand.
ASCIA resources are based on published literature and expert review, however, they are not intended to replace medical advice. The content of ASCIA resources is not influenced by any commercial organisations.
For more information go to www.allergy.org.au
To donate to immunology/allergy research go to www.allergyimmunology.org.au
Updated September 2022
![]() ASCIA Allergic Rhinitis Treatment Plan 2024175.28 KB
ASCIA Allergic Rhinitis Treatment Plan 2024175.28 KB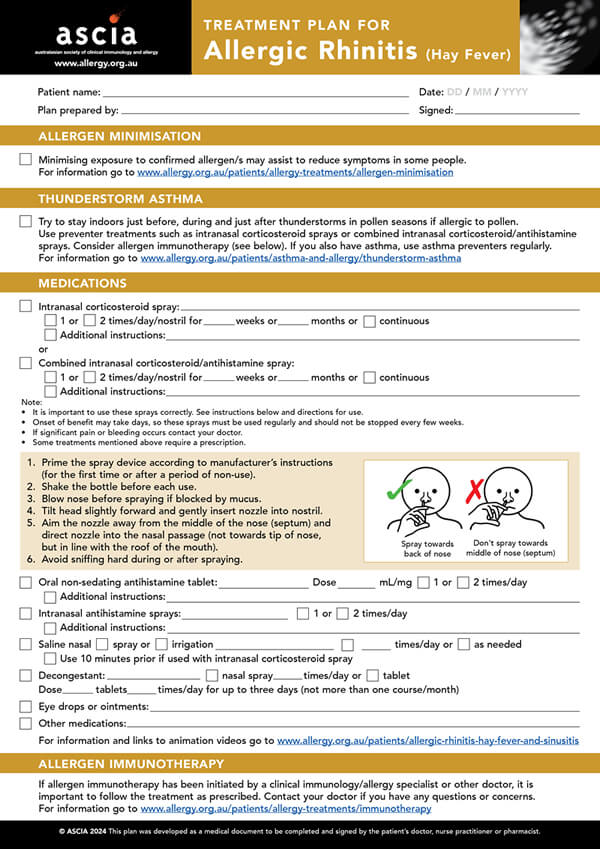

 Allergic rhinitis (hay fever) is very common and is caused by the nose and/or eyes coming into contact with allergens in the environment. These include pollens (from grasses, weeds or trees), dust mites, moulds and animal dander (skin flakes from animals with fur). Allergic rhinitis can cause a runny, itchy or congested nose, sneezing and itchy/watery eyes. These symptoms may be mistaken for infections such as colds and flu, but treatments are different. Sinusitis can occur if allergic rhinitis is not treated correctly.
Allergic rhinitis (hay fever) is very common and is caused by the nose and/or eyes coming into contact with allergens in the environment. These include pollens (from grasses, weeds or trees), dust mites, moulds and animal dander (skin flakes from animals with fur). Allergic rhinitis can cause a runny, itchy or congested nose, sneezing and itchy/watery eyes. These symptoms may be mistaken for infections such as colds and flu, but treatments are different. Sinusitis can occur if allergic rhinitis is not treated correctly. 